Which way is the best and how to reverse your cavities?
Wouldn’t it be great—a miracle—if decayed teeth were alive and could regrow? They are and they can. Why aren’t dentists writing about this? It is hardly perhaps in dentists’ best interests to share the least intrusive dental interventions when this is their bread and butter but we think we have found an exception to this rule, below! This in-depth researched and referenced long-form article may not only save your teeth, but save you a fortune on unnecessary dental bills!
Word count: 5000 words
Reading Time: 21mins
I had an emergency tooth extraction after a year of excruciating pain at a British dental hospital because of a cavity, there were no NHS places at any local dentists and I couldn’t afford to go private.
“A report from the watchdog Healthwatch England in 2019 found that 85% of dental practices were closed to new NHS adult patients and 40% were closed to new NHS child patients.”
It isn’t just the UK where poverty may be a social factor resulting in poor access to dental treatment, and potentially untreated dental caries, in the US almost half of adults in households earning less than $10,000 had untreated dental caries, compared to one in six adults in households earning less than $35,0001.
A few months later I suddenly felt pain in another tooth and I was terrified because my precarious financial situation hadn’t changed and I feared another year of agony and being left toothless again if I didn’t find a better way and do some research urgently.
This article is about which way is the best, and how, to reverse your cavities based on the latest research in case you are in, or ever face, the same predicament, in a more cost-effective way than mechanical intervention by a dentist, even if you could afford one!
This post is available free for three months and then it will be archived. You can gain access to the full archive for £5/month, and unsubscribe anytime, or £50/year. If you are low/no income just drop me a line at mark dot holmes at whichwayhow dot com and I’ll drop you a comp. paid sub, no questions asked!
KEY FINDINGS
1. Dental caries is a transmissible, and reversible, bacterial disease not just a hole in the teeth requiring mechanical repair.
2. White spots on your teeth are an Early Warning Sign you have the disease. But there’s still time to reverse the process of the disease at this point, because teeth can grow back.
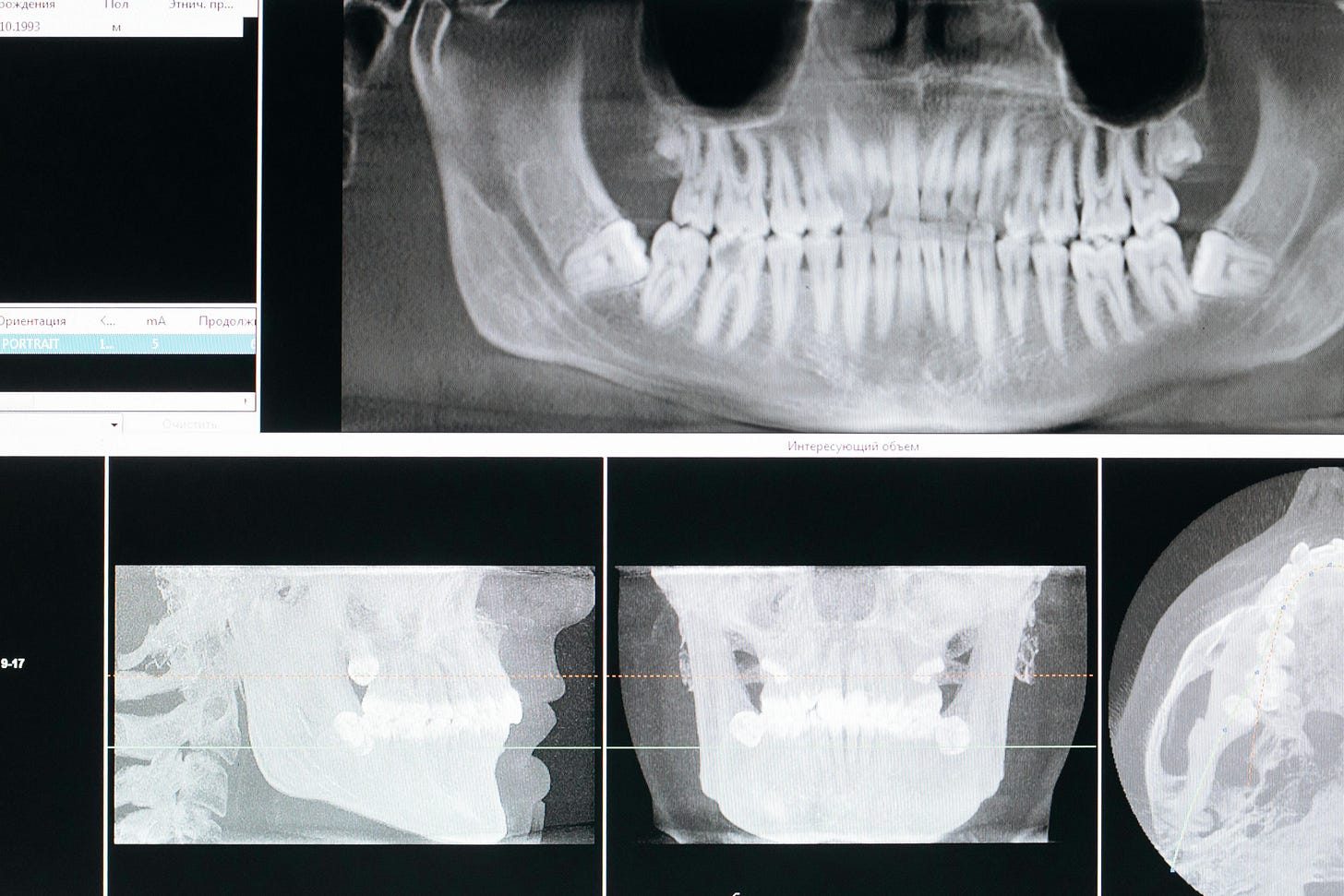
3. The disease progresses when the three pathological factors (acid-producing bacteria; fermentable carbohydrates; and dysfunctional saliva flow) exceed the three protective factors (saliva components and flow; fluoride; and antibacterial therapy.) A minimum of 6.5mg to 10mg of Xylitol daily can remove acid-producing bacteria from the mouth completely in six months.
4. Your dentist should offer you a 3 vs 3 concept risk assessment eg. CAMBRA, to address the disease and offer the least invasive mechanical procedures.
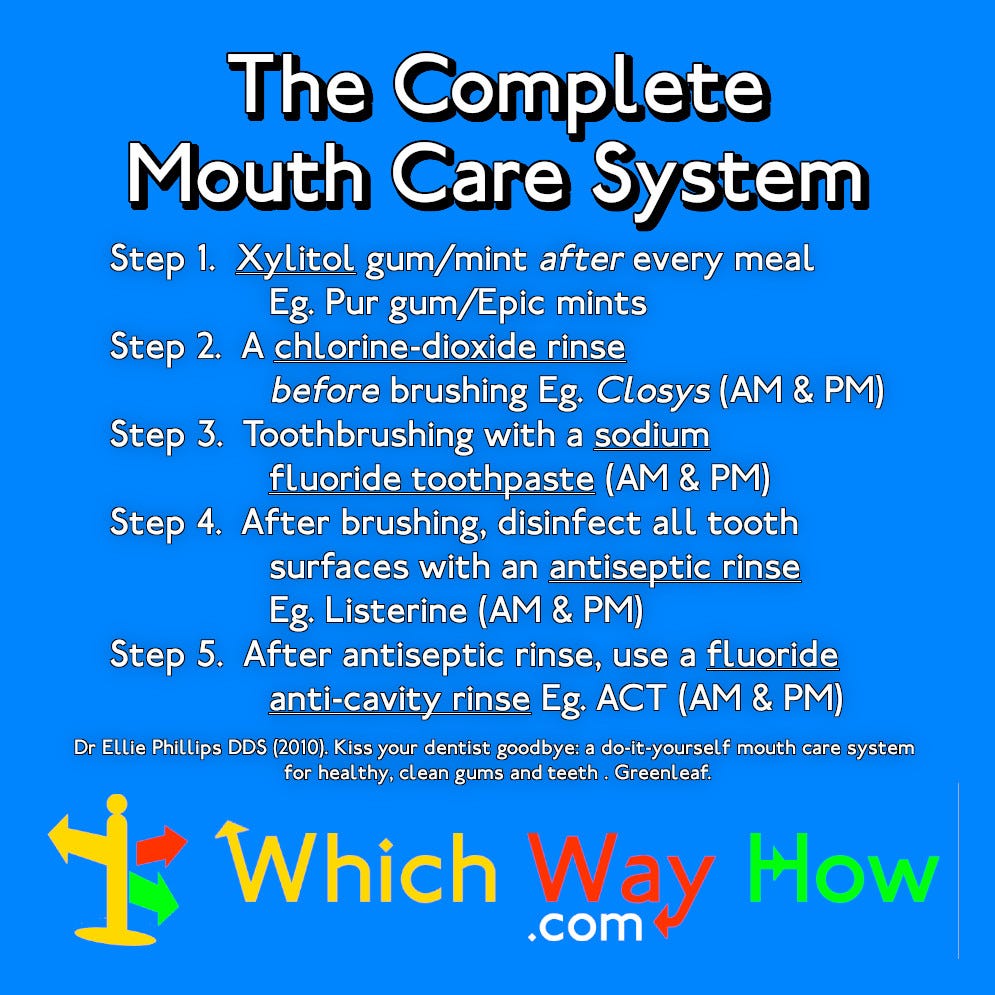
5. Dr Ellie Phillips’ Complete Mouth Care System addresses all the protective factors in five steps: 1. Xylitol; 2. A chlorine-dioxide rinse before brushing; 3. Toothbrushing; 4. Disinfect all tooth surfaces with antiseptic rinse; 5. Fluoride anti-cavity rinse. I give her recommended products at the end and the ones I personally substitute.
What causes tooth decay?
Dental caries, or tooth decay, as it is popularly known, is often wrongly thought of as holes in the teeth requiring mechanical repair, rather than as symptoms of a disease requiring multi-faceted treatment of the causes, or other teeth will be similarly affected as the disease spreads. This is why it is not surprising for other cavities to develop after you have ‘fixed’ the first.
“Clinical dentistry, even today, generally considers that placing a restoration “fixes” dental caries. Unfortunately, placing the restoration only removes the offending bacteria from that cavity in that tooth. It does not deal with the disease in the rest of the mouth.”2
This popular misconception seems compounded by dentists immediately advocating expensive invasive surgery as a solution rather than the minimum invasive treatment possible, which studies have shown is a better way.3
“Although dental caries is the most prevalent infectious disease in humans, affecting 97% of the population in their lifetimes, we primarily treat the effects of dental caries, and not the disease itself.” 4
It is shocking how many cases of dental caries remain untreated: Over a quarter of 20–64-year-olds had untreated dental caries in the US from 2015-2018.
It was slightly worse in the UK in 2018, where 27% of the adult population had untreated tooth decay on an average of two teeth.
Before we consider the best way of self-treating cavities, and how to reverse cavities, we need to briefly understand what causes tooth decay.
(H2) The 3 vs 3 Concept “Caries balance” between pathological and protective factors
Dental caries is a dynamic disease which proceeds when the balance between pathological (abnormal/disease) factors exceeds the protective factors in the mouth.
“Dental caries progression or reversal depends upon the balance between demineralization and remineralization and can be visualized for clinical purposes as the "caries balance." This balance is determined by the relative weights of the sums of pathological factors and protective factors.”5 [My bold]
Pathological Factors
The three most important pathological factors which threaten our teeth are:
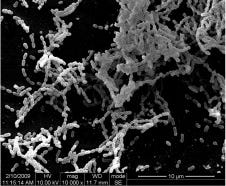
1. Acid-producing bacteria Eg. The three most serious offenders sound like dinosaurs and look like alien worms in microscopic form: Streptococcus mutans (the worst culprit. see below!); Streptococcus sobrinus; and the lactobacilli species.
(N.B. Not all bacteria in your mouth are acid-producing, though, most are good (!) and you need the good bacteria, which is why coconut oil pulling, which destroys all bacteria, may do more harm than good!)
When these acid-producing bacteria make contact with sugars and starches from foods and drinks—see next pathological factor—they form a sticky acidic film (biofilm) which we know as dental plaque. This accumulates on the tooth surface and attacks the tooth’s enamel causing a loss of minerals, or demineralisation. (If plaque is not removed by your toothbrush or flossing it will form tartar which can only be removed by your dentist.)
Unless this is countered by sufficient protective factors, see below, demineralisation can lead to a white spot on the teeth, which is a sign of a lesion/cavity inside the tooth. However, what your dentist might not explain is that this can be reversed by remineralisation rather than expensive invasive mechanical treatment.
2. Fermentable carbohydrates Eg. Sucrose, glucose, fructose and cooked starch are pathological factors which when combined with acid-producing bacteria cause dental caries.
Therefore, the avoidance of sugary, starchy food and drink, and replacing these, or finishing a meal, with teeth-friendly alkaline alternatives such as milk, cheese, and even dark chocolate may help. 6
Dark chocolate is a surprising one, but this is based on using one high in Cocoa, because the polyphenols in cocoa can help reduce the growth of Streptococcus mutans. 7
Therefore, avoiding carbohydrates on a keto diet may even help reduce cavities, as well as reduce your waistline!
3. Dysfunctional saliva flow is another pathological factor. Eg. Dry-mouth, medically called xerostomia.
“Chronic xerostomia significantly increases the risk of experiencing dental caries, demineralization, tooth sensitivity, candidiasis and other oral diseases that may affect quality of life negatively.” 8
Having a dry mouth is common the ‘morning after’ a heavy night of drinking because alcohol is a diuretic and can also change your salivary flow rate9 . Therefore, avoiding alcohol, and other diuretics, like coffee, can reduce dry mouth.
If the suggestion of avoiding alcohol is problematic—a quick plug—I am an addiction counsellor when I am not doing this, and recommend my book, “Holmes’s Complete Guide To Stop Drinking Alcohol; the easy, mindful and pain-free way” with over 300 academic references to help avoid alcohol altogether, or reduce alcohol intake, easily, available at all good retailers (End of plug!).
But dry mouth can also be a side-effect of medication or medical intervention, which may be more difficult to avoid. After I quit drinking, I was on anti-depressants (nobody mentions that drinking causes anxiety and depression and/or the fact that many, like I, used alcohol to self-medicate), and I often still had dry mouth. This was a year or two before I needed emergency dental treatment, which may have been due to my alcoholism, or medication, causing xerostomia.
Protective Factors
And the three most important protective factors we need to continuously counter those pathological factors are:
1. Saliva components and flow. Saliva helps to remove carbohydrates from the plaque; provide proteins and lipids to form the protective pellicle (thin layer around the tooth surface); calcium and phosphate; and anti-bacterial proteins.10 If you have dry mouth this will reduce the saliva, tipping the balance in favour of the pathological factors, and cause cavities.
To relieve the discomfort of dry mouth, the American Dental Association recommends avoiding alcohol, limiting caffeine intake, sipping water, using an alcohol-free mouth rinse and chewing sugar-free gum to stimulate saliva production.
2. Fluoride. Eg. Fluoride toothpaste/mouthwash/varnish. Fluoride, calcium and phosphate are the key ingredients for remineralisation.
But be careful because not all fluorides are the same, and one type of fluoride, Stannous Fluoride—even found in a popular brand of toothpaste which shall remain nameless— causes brown staining, which is a high price to pay for preventing cavities. So please check the ingredients of your toothpaste!
“Stannous fluoride was popular in the 1960s because it was shown to reduce gum inflammation. The problem with stannous fluoride, however, is that it creates unattractive black or brown staining on teeth.”11
Fluoride varnish is particularly useful for children, and I have used it with my own children. It is painted onto children’s teeth (aged 0-18) by a dentist twice to four times a year and slowly releases fluoride to prevent tooth decay.
“The review suggests a substantial caries‐inhibiting effect of fluoride varnish in both permanent and primary teeth” ]
3. Antibacterial therapy. Saliva is a natural anti-bacterial therapy but insufficient if pathological factors outweigh protective factors. An anti-bacterial mouthwash can help reduce harmful bacteria. But not all anti-bacterial mouthwashes are equally effective against all acid-producing bacteria.
For example, Chlorhexidine, available in a mouthwash form, effectively reduces mutans streptococci levels, but it is not so effective against the lactobacilli species. We will consider the most effective mouthwash shortly.
However, mouthwashes are not the only anti-bacterial therapy, and Xylitol, see more below, available as a mint or gum, can also reduce bacterial adherence and transmission of mutans streptococci, and a prospective study in Finland suggests it may be more effective than fluoride varnish or chlorhexidine.12 Chewing gum can also stimulate salivation to relieve dry mouth.
Probiotic Bacteria
Another possible alternative to antibacterial therapy, which I have not tried but I believe is at the cutting edge of research and may help you, is Probiotic bacteria, particularly with new awareness of the importance of the ‘second brain’ of the gut:
“The enteric nervous system that regulates our gut is often called the body’s “second brain.” Harvard Medical School13
Probiotics means “for life” and Probiotic bacteria is defined as, “live microorganisms which, when administered in adequate amounts, confer a health benefit on the host” 14 and they can be found naturally or genetically engineered.
Research has found that certain probiotic bacteria can help prevent or treat tooth decay. These probiotics include Lactobacillus (such as salivarius, reuteri, and rhamnosus) and Bifidobacterium, which are naturally found in the mouth. They help by:
1. Reducing Harmful Bacteria: They decrease the number of harmful bacteria like Streptococcus mutans, which is a major cause of cavities.
2. Inhibiting Bacterial Virulence: They target specific genes in Streptococcus mutans that are responsible for making it more harmful. By interfering with these genes, such as GtfB and LuxS, probiotics can disrupt the bacteria's ability to form biofilms and cause tooth decay.
This means that probiotics can make it harder for Streptococcus mutans to thrive and damage teeth, thereby reducing the risk of cavities.
Probiotic bacteria can be administered in a variety of forms including dairy products, ice cream and curds, oral thin film, tablets and lozenges15 eg. PerioBalance, see picture below, which contains patented (although I don’t know how you can patent a bacteria!) active Limosilactobacillus Reuteri Prodentis® (formerly known as Lactobacillus reuteri Prodentis®).

Caries Risk Assessment
Having considered the 3 pathological factors and 3 protective factors, isn’t this something your dentist should also be considering with you in their caries risk assessment? Or is this the first time you’ve come across this? It was for me. And yet multiple medical studies state:
“The 3-vs-3 concept should be the first step in providing a risk assessment and an understanding of the caries process as it is progressing in an individual patient.”16
“A structured caries risk assessment should be carried out based upon the concept of the caries balance. Following the risk assessment a treatment plan is devised which leads to the control of dental caries for the patient.” 17
Therefore, dentists should start by doing a risk assessment with the patient to analyse the extent of the pathological and protective factors in your mouth—the 3-vs-3 concept, or, similar, for example, CAMBRA, which stands for "Caries Management by Risk Assessment"—and yet I have never completed a questionnaire or witnessed this approach being used in the UK for my children, wife or I in any dental clinic or dental hospital in over 50 years.
The Complete Mouth Care System
If you are self-treating tooth caries, like me, the best way I have found, and use myself, which addresses all the protective factors, (and I receive no sponsorship or financial incentive for recommending this) is Dr Phillips’ Complete Mouth Care System as described in her book, “Kiss your dentist goodbye” and you can also find her describing this in an hour-long video on YouTube here.
I have adapted this system to be more affordable and, potentially more effective, and written to Dr Ellie three times for her response but had no reply from the contact page on her website. I have also left a link to this deep dive in the comments of her video which she has removed.
In order to be balanced, you can find “a deep dive on @dr.elliephillips,” on YouTube here, which claims to consider, “The good, the bad and the ugly of Dr Ellie Phillips,” although Paul eventually concludes she is an “idealist saint.”
Criticism of Dr Ellie Phillips and the Complete Mouth Care System
Let’s look at Paul’s key criticisms upfront first:
1) Cost. The system costs around $500 USD/year, which is a fair estimate, even on the low side for the UK.
2) Gatekeeping. Paul claims Dr Phillips, “gatekeeps her knowledge of how to use the system”. He quotes her course and shows the fee of $98 and her book. There is some truth to this if he is referring to her sharing an evidence base, but she does refer to this in her book, although obviously you need to buy this book (£3.49 for kindle edition). And it would be nicer if the research was freely available, but you could use a library.
3) Financial incentive. Paul claims Dr Ellie has a company that makes mints and gums which uses her system, which is true (I suggest alternatives, though, below, because her ‘Zellies’ are expensive.)
Paul also states, “she gets a kickback from all the products that she has put into her complete mouthcare system.” It is true her system contains branded products which her company redistributes but I don’t know how Paul knows the financial arrangement between them.
Paul also criticises her for using Amazon affiliate links, (which I can’t, because I do too!) but these are at no cost to the consumer and therefore I think it is a little bit harsh. Paul then says, “Personally I don’t think that it’s such a bad thing to have a financial incentive” when he has just titled this section, “The bad,” but explains he feels like he is “being sold to so hard when I’m looking at her content.”
But this seems like a judgment of style over substance, and I personally love her style, and Paul’s too! But shouldn’t we be focusing on the content? He comes to that next.
4) Validity. Paul criticises Dr Phillips for not providing evidence to back up her claims using the example of her video, “How to REGROW Receding Gums” in which she states that you should not blame gum recession on toothbrushing or grinding teeth.
Paul quotes one study, “Evaluation of gingival recession in left- and right-handed adults”, and links to it in his notes, which suggests evidence of toothbrushing technique affecting gingival recession, and another study, “Gingival recession: its causes and types, and the importance of orthodontic treatment” suggesting “V-shaped local retraction is associated with teeth subjected to occlusal trauma, especially in patients with bruxism and clenching habits.”
However, the first study had a sample size of 110 which is too small to necessarily draw wider conclusions from, and the second study stated, “Clinical as well as experimental trials on the subject would help to clarify this matter, of which understanding is not very deep in the related literature.” [my italics].
Also, and possibly the most important thing, this does not necessarily negate the argument in Dr Phillips’ video, which is that it wasn’t the toothbrushing, but “something else occurred to make your gums recede. [7:19]… the first thing to think about is how acidic is your mouth and for how long every day [8:00].” This is perfectly correct, and Paul should know that, particularly if he has read both her books as he claims.
To be fair to Paul, Dr Phillips doesn’t give any links to research evidence below her video, which is a pity, but she is right about the fundamental point which Paul seems to be missing.
Paul continues to criticise her for stating on her website that, “There are no conclusive studies to show flossing or tongue scraping are superior to good brushing,” and then quotes a study, “The Comparative Evaluation of the Effects of Tongue Cleaning on Existing Plaque Levels in Children,” which states, “Tongue scraping and tongue-brushing groups showed statistically significant reductions in plaque levels after 10 days and also after 21 days,” based on a sample of 45. I don’t understand how Paul regards a study with a sample size that small as being conclusive, either way!
And Paul fails to consider the reason for Dr Phillips stating this in the first place, which is because of the danger of mechanical intervention transmitting bacteria, which she does source on her website, although this was admittedly a case study of only one 59-year-old lady.
Paul finally comes to what he calls “the Ugly: Good and Bad Bacteria.” He states, “there aren’t really any good bacterias [sic] in your mouth.”
However, according to a study, “Oral microbiome: Unveiling the fundamentals” there are over 700 different species of bacteria and some, the commensal populations, are ‘good bacteria’ in the sense they do not cause harm and stop the pathogenic species from sticking to the mucosa:
“The oral cavity has the second largest and diverse microbiota after the gut harboring over 700 species of bacteria… There is a symbiotic relationship between the microorganisms in our oral cavity based on mutual benefits. The commensal populations do not cause harm and maintain a check on the pathogenic species by not allowing them to adhere to the mucosa. The bacteria become pathogenic only after they breach the barrier of the commensals, causing infection and disease.”
Therefore, I don’t understand how Paul can state there are no good bacteria in your mouth. The study he cites, “The power of saliva: Antimicrobial and beyond” which explains how saliva plays a role in managing the attachment and colonization of bad bacteria in the mouth:
“Saliva plays a dual role in modulating microbial attachment and colonization in the mouth. Dental enamel is coated with a film of salivary pellicles and proline-rich proteins, which bacteria (such as Streptococcus gordonii, Actinomyces naeslundii, and Porphyromonas gingivalis and yeasts) exploit as receptors to adhere to dental surfaces and avoid elimination.”
I have explained the number one importance of saliva and salivatory flow in Protective Factors, above, and Paul should also be aware of the importance Dr Phillips attaches to this as she states in her book:
“Strong, healthy teeth need to be bathed regularly in mineral-rich saliva in order to naturally repair tooth defects and weaknesses. Xylitol stimulates mineral-rich saliva to flow into the mouth.”
And Dr Phillips provides a clear source for this: O. Aguirre-Zero, D. T. Zero, and H. M. Proskin. “Effect of Chewing Xylitol Chewing Gum on Salivary Flow Rate and the Acidogenic Potential of Dental Plaque.” Caries Research 27 (1993): 55–59.
In Dr Phillips’ comment on Paul’s post, Dr Phillips defends her integrity and the Complete Mouth Care System against these criticisms assuring him of her valid credentials, and most importantly, willingness to have her system tested:
“This is Dr. Ellie and I would like to thank you for making this video. My system was developed by trial and error - not assessing studies - in the 1970s and now there have been five decades using power-point presentations in pre-natal clinics, libraries, hotel ballrooms, in small groups for oncologists, nurses, at hygienist conferences, and independent pharmacies - for zero financial reward - at a time when I could have been filling and restoring teeth - instead of teaching people how to avoid dental problems. I have tried to run studies on my system - but have had zero interest from universities, dental insurance companies or any other outlet - which is why there are no studies on my system at this point.
“Also, this system is the only way I KNOW to get people out of trouble - the one way that works. I specialized in both padiatric and geriatric dental fields - so I have a wider vision of dentistry than many. Senior dental spending in the United States shows the appalling outcome of following other methods. Thanks again.”
I think Dr Phillips sums up the biggest criticism of her system herself, which is that there is no independent research of the effectiveness of the ‘Complete Mouth Care System’, as a system, but I will try to provide studies that support the parts, to enable you to evaluate it yourself, below.
When I left comments on her YouTube video, and Paul’s, to be fair, to address the criticisms, with a link to this article to respond, they BOTH deleted them. I can only conclude that perhaps Dr Phillips’ overriding concern is a financial incentive, and perhaps Paul can only give criticism and not take it!!!
What does the Complete Mouth Care System claim to do?
First, the Complete Mouth Care System claims to enhance the protective factors in a process or sequence to, “stop oral health problems, prevent and reverse gum recession, plaque, cavities and create clean, white and healthy teeth.”18
To save you time, here is a summary of the steps Dr Phillips recommends:
I will now explain the main elements of the Complete Mouth Care System in more detail, the supporting independent evidence and the best products, in terms of value for money, so you don’t need to necessarily watch the video or buy her book, like I have, both of which I recommend by the way, or take her course, which I haven’t.
Step 1. Xylitol
We have already discussed how chewing an alcohol-free gum can relieve dry mouth symptoms, and how xylitol can also reduce bad bacteria.
In terms of dosage, a minimum of 6.5mg to 10mg of Xylitol daily can remove acid-producing bacteria from the mouth completely in six months.19
Dr Phillips specifically recommends her own xylitol products called “Zellie’s” mints (0.5 xylitol/piece) or gums (1g xylitol/piece) after every meal, two pieces of gum, five times a day. But these are expensive, and hard to get in the UK.
However, I found Pür 100% xylitol chewing gum (1g/piece) and Epic 100% Xylitol gum/mints (0.5g/ piece) easily available in the UK and slightly cheaper. I use Pür spearmint gum (2 pieces =2g) and give Epic mints to my kids.
But to meet the minimum effective dosage, this means I would need to take three and a half servings daily, which isn’t too bad, but my kids would need six servings, which is obviously more than after every meal, and very expensive.
So, what we do, which may potentially make the Complete Mouth Care System more effective, as well as being the cheapest way of doing it, is use one teaspoon (4mg) of powdered Xylitol on sugar-free muesli in the morning, and then supplement this with gum/mints after lunch and dinner. The brand I use is called ‘Nature Diet - Xylitol 1 kg’ from Amazon.co.uk (currently £6.82).
Step 2. A chlorine-dioxide rinse before brushing.
In her book, Dr Phillips recommends Closys in the United States, or Ultradex in the UK. Don’t use the flavouring that comes with it because in her book, Dr Phillips says this reduces its effectiveness.
I use Ultradex and I find it removes all the bits of food in my last meal very effectively.
Step 3. Toothbrushing
Dr Phillips claims there is no research on the best brush to use, but the bristles must have rounded ends, and not be too hard or stiff, to avoid damaging the gums, changed every three months, and be disinfected daily with a ½ ounce of Listerine mouthwash for 30 seconds.
I didn’t consider disinfecting my toothbrush before this, but Dr Phillips explains that any infection can easily remain on your toothbrush and reinfect the mouth, and also other toothbrushes if kept nearby, so don’t keep your toothbrush near or in the same container as other family members, and let your toothbrush dry completely before re-using, so I have two, one for morning and one for nighttime use.
Another useful tip Dr Phillips shares is not to keep your toothbrush on a surface near a toilet, because a study shows flushing an open toilet can transmit harmful bacteria to your brush. This is worth knowing because every house I have ever lived in has a sink next to the toilet!
Toothpaste
Dr Phillips specifically recommends Crest Cavity Protection regular toothpaste which has Sodium Fluoride 0.243%, 2.43mg/g, (0.15% w/gv fluoride ion [which I found is equivalent to 1500ppm]). But, be careful, because not all Crest toothpastes have this formulation, and some include stannous fluoride.
Another study I found said that 1450 to 1500 ppm (parts per million) is the optimum level of fluoride in toothpaste for reducing caries:
“We found that there was less new decay when toothbrushing with toothpaste containing 1000 to 1250 ppm or 1450 to 1500 ppm fluoride compared with non‐fluoride toothpaste, and that toothbrushing with 1450 to 1500 ppm fluoride toothpaste reduced the amount of new decay more than 1000 to 1250 ppm toothpaste.” 20
This is also the toothpaste Dr Phillips recommends and it is not the cheapest toothpaste on the market in the UK, about £6, but it is 232ml, which is twice the size of my regular one for half-the-price.
However, there is a potentially more effective toothpaste to use in the Complete Mouth Care System to rebuild tooth enamel.
I uncovered a study called, “Mode of action studies on the formation of enamel minerals from a novel toothpaste containing calcium silicate and sodium phosphate salts” which found that when Calcium silicate is deposited onto enamel surfaces from a new toothpaste formulation, it can form the enamel mineral hydroxyapatite (HAP), effectively rebuilding enamel as strong as the enamel underneath:
“A novel toothpaste formulation containing CaSi can form HAP on enamel surfaces. The potential of this technology is for a novel approach to the repair of demineralised enamel and the protection of enamel during acid exposure.”
This “novel toothpaste” is called “Regenerate Advanced Toothpaste” and although it is expensive it is the only toothpaste that I have found that is supported by research which demonstrates that it can rebuild enamel.
However, it is important to consider a) whether Regenerate meets the criteria for fluoride ppm of the other toothpaste recommended, and b) whether there are any possible contraindications from using this alongside the other mouthwash formulations in the system:
a) Regenerate’s stated ingredients are: Aqua, Hydrogenated Starch Hydrolysate, Peg-40 Hydrogenated Castor Oil, Glycerin, Tetrapotassium Pyrophosphate, Citric Acid, Sodium Benzoate, Aroma, Phenoxyethanol, Sodium Lauryl Sulfate, Trisodium Phosphate, Cocamidopropyl Betaine, Sodium Saccharin, Sodium Fluoride, Limonene, CI 42090, CI 47005. And Unilever has confirmed that it has 1450 parts per million of Sodium Fluoride which meets the criteria of the recommended amount in the study above.
b) Unilever have also confirmed that there are no contraindications from using Regenerate alongside other mouthwashes, so it may be an effective modification to the Complete Mouth Care System, alongside the other products recommended here. However, I wish to emphasise, this has not been endorsed by Dr Phillips.
Step 4. Disinfect all tooth surfaces with antiseptic rinse
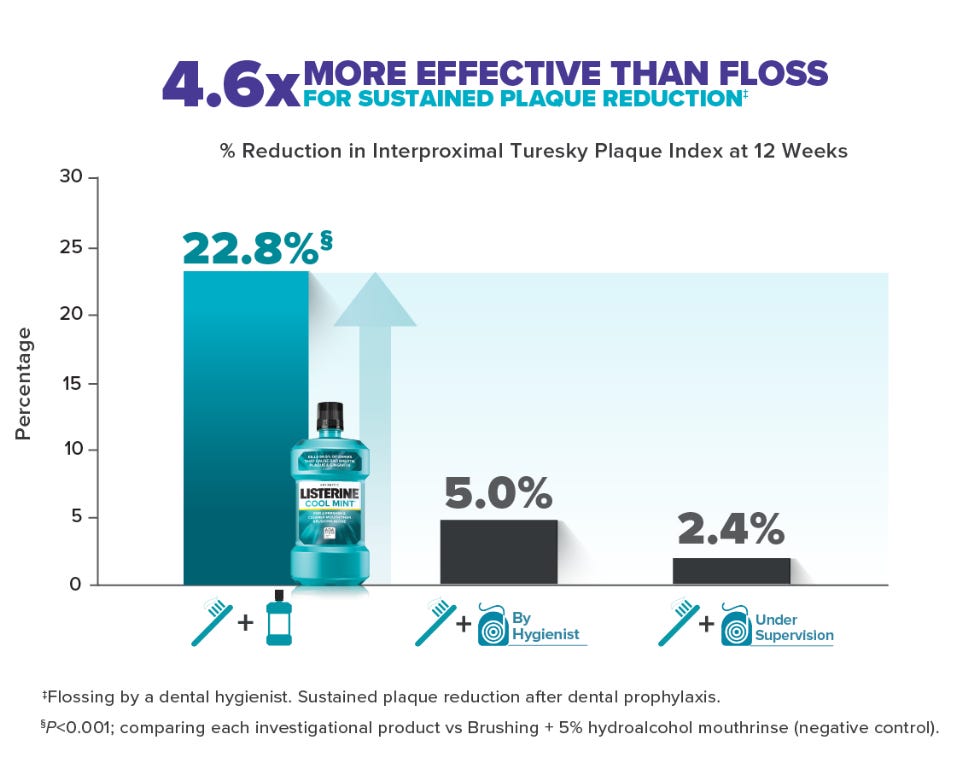
Dr Phillips calls this a ‘liquid floss’, and claims rinsing with Listerine twice a day is as effective as flossing once a day (she is against flossing by the way because it can damage gums) and there is research to support this. Listerine contains menthol, thymol, eucalyptus oil and methyl salicylate—a four essential oil (4EO) mouthwash—which has been found to be effective:
“Rinsing with a 4EO mouthrinse statistically significantly improved all oral health outcome measures at all time points compared to a NC [negative control 5% hydroalcohol] rinse in this 12-week clinical trial. While professional and supervised flossing improved gingival health compared to use of the NC rinse, statistically significant plaque reduction with dental flossing was not attained at the end of the 12-week trial.” 21
If you are anything like me and hate flossing, even if I could (!), then you will love the fact that a 4EO mouthwash, like Listerine, is more effective!
Dr Phillips specifically recommends Listerine Original or Listerine Cool Mint—which is the one I use because it’s cheaper—and none of the other Listerine mouthwashes.
She also suggests what I call, ‘resistance training’, and to gradually build up how long you rinse with it for, which isn’t easy, because this stuff is really, kind of, ‘ultra-fresh’, in a good way, but my tolerance has increased and I always feel better afterwards. At least, as soon as I have had the final mouthwash after it which we will come to next.
Step 5. Fluoride anti-cavity rinse
Finally, Dr Phillips recommends a 0.05 percent sodium fluoride rinse to strengthen tooth enamel. The specific brand she recommends is “ACT anticavity rinse”, but in her video she is very particular about it being the regular size, not the larger “restoring” version which states on the back it is only 0.02% sodium fluoride. Also, be careful to get the green one, like the one in the picture below—not the blue one—because the green one is alcohol-free.
However, ACT is very expensive in the UK, and I found a cheaper 0.05 percent sodium fluoride alcohol-free rinse in the UK called Colgate Fluorigard, see picture below (and green one, too!) which is what I use.
Conclusion
Discovering that tooth decay was a curable disease and could be self-treated saved me when I couldn’t afford a dentist.
This self-treatment isn’t free, but it is potentially cheaper than dentists’ invasive mechanical treatment, particularly when some dentists don’t even conduct a 3 vs 3 concept ‘caries balance’ risk assessment, which could therefore lead to more unnecessary mechanical treatment.
Next time you visit your dentist, demand a 3 vs 3 concept ‘caries balance’ risk assessment, or CAMBRA, before you let them do anything mechanical! If they don’t know what it is, which they should do, show them this article and the research evidence.
After six months of using, I stress, my version of the Complete Care Mouth System, I cannot say my teeth are much whiter than they were before, but that could be due to reduced enamel, and/or smoking and drinking for many years. However, they do feel a lot smoother and they do visibly glint in the light. More importantly, I have no pain in my teeth and no teeth removed since that last one.
I plan to switch to Regenerate toothpaste, to try and rebuild the enamel on my teeth, and I will update this article accordingly if there is any improvement.
I hope this article saves you time and money, and has provided a workable best way solution, and if so, please share it to help your friends.
Update 23rd August 2024
Please consider a Vitamin D supplement, especially if you do not get adequate exposure to the sun, as research suggests Vitamin D deficiency may also be linked to cavities.
"Vitamin D deficiency is linked to cavities: Studies have shown that a vitamin D deficiency is associated with an increased risk of tooth decay in children and adults."22
If you’d like to buy me a coffee you can do so below:
And if you don’t want to miss the next deep dive in a fortnight—which may be just what you need to solve your problem—subscribe for FREE below (No paid option, Whichwayhow.com is always free!)
If you enjoyed this post, you may also enjoy: Whichwayhow to do Breathwork, Whichwayhow to Journal, Whichwayhow to Reverse Cavities and Whichwayhow to be a hero (of the everyday!)
References
15. Dye BA, Thornton-Evans G. Trends in oral health by poverty status as measured by Healthy People 2010 objectives. Public Health Rep. 2010 Nov-Dec;125(6):817-30. doi: 10.1177/003335491012500609. PMID: 21121227; PMCID: PMC2966663. [ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2966663/]
Featherstone JD. Dental caries: a dynamic disease process. Aust Dent J. 2008 Sep;53(3):286-91. doi: 10.1111/j.1834-7819.2008.00064.x. PMID: 18782377.
Phillips, Ellie. Kiss Your Dentist Goodbye: A Do-it-yourself Mouth Care System for Healthy, Clean Gums, and Teeth. Greenleaf, 2010
Berg, J.H. The Marketplace for New Caries Management Products: Dental Caries Detection and Caries Management by Risk Assessment. BMC Oral Health 6 (Suppl 1), S6 (2006). https://doi.org/10.1186/1472-6831-6-S1-S6
Conference paper. Caries Prevention and Reversal Based on the Caries Balance. John D.B. Featherstone, MSc, PhD. Pediatr Dent 2006;28:128-132. And see, Featherstone JDB. The science and practice of caries prevention. J Am Dent Assoc 2000;131:887-899.
Phillips, Ellie. Kiss Your Dentist Goodbye: A Do-it-yourself Mouth Care System for Healthy, Clean Gums, and Teeth. Greenleaf, 2010
Ferrazzano, G. F., Amato, I., Ingenito, A., De Natale, A., & Pollio, A. (2009). Antimicrobial activity of polyphenols extracted from cocoa and their effect on mutans streptococci. Journal of Agricultural and Food Chemistry, 57(21), 10132-10138. doi:10.1021/jf902062x
Plemons J.M. Al-Hashimi I. Marek C.L. American Dental Association Council on Scientific Affairs. Managing xerostomia and salivary gland hypofunction: executive summary of a report from the American Dental Association Council on Scientific Affairs. JADA. 2014; 145: 867-873
Inenaga K, Ono K, Hitomi S, Kuroki A, Ujihara I. Thirst sensation and oral dryness following alcohol intake. Jpn Dent Sci Rev. 2017 Aug;53(3):78-85. doi: 10.1016/j.jdsr.2016.12.001. Epub 2017 Feb 27. PMID: 28725298; PMCID: PMC5501731. See also, da Silva L. Kupek E. Peres K.G. General health influences episodes of xerostomia: a prospective population-based study. Community Dent Oral Epidemiol. 2017; 45: 153-159.
Featherstone JD. Dental caries: a dynamic disease process. Aust Dent J. 2008 Sep;53(3):286-91. doi: 10.1111/j.1834-7819.2008.00064.x. PMID: 18782377.
Phillips, Ellie. Kiss Your Dentist Goodbye: A Do-it-yourself Mouth Care System for Healthy, Clean Gums, and Teeth. Greenleaf, 2010
Lynch H, Milgrom P. Xylitol and dental caries: An overview for the clinician. J Calif Dent Assoc 2003;31:205-209. And see, Anderson, M. (2003). Chlorhexidine and xylitol gum in caries prevention. Special Care in Dentistry.
“The Gut and the Brain” Harvard Medical School website accessed on 16thJuly 2024. https://hms.harvard.edu/news-events/publications-archive/brain/gut-brain
Fijan S. Microorganisms with claimed probiotic properties: an overview of recent literature. Int J Environ Res Public Health. 2014 May 5;11(5):4745-67. doi: 10.3390/ijerph110504745. PMID: 24859749; PMCID: PMC4053917.
Abou Neel EA, Aljabo A, Strange A, Ibrahim S, Coathup M, Young AM, Bozec L, Mudera V. Demineralization-remineralization dynamics in teeth and bone. Int J Nanomedicine. 2016 Sep 19;11:4743-4763. doi: 10.2147/IJN.S107624. PMID: 27695330; PMCID: PMC5034904. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5034904/ ]
Conference paper. Caries Prevention and Reversal Based on the Caries Balance. John D.B. Featherstone, MSc, PhD. Pediatr Dent 2006;28:128-132. And see, Featherstone JDB. The science and practice of caries prevention. J Am Dent Assoc 2000;131:887-899.
Phillips, Ellie. Kiss Your Dentist Goodbye: A Do-it-yourself Mouth Care System for Healthy, Clean Gums, and Teeth. Greenleaf, 2010
Phillips, Ellie. Kiss Your Dentist Goodbye: A Do-it-yourself Mouth Care System for Healthy, Clean Gums, and Teeth. Greenleaf, 2010
Phillips, Ellie. Kiss Your Dentist Goodbye: A Do-it-yourself Mouth Care System for Healthy, Clean Gums, and Teeth. Greenleaf, 2010
Walsh T, Worthington HV, Glenny AM, Marinho VC, Jeroncic A. Fluoride toothpastes of different concentrations for preventing dental caries. Cochrane Database Syst Rev. 2019 Mar 4;3(3):CD007868. doi: 10.1002/14651858.CD007868.pub3. PMID: 30829399; PMCID: PMC6398117. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6398117/
Bosma ML, McGuire JA, Sunkara A, Sullivan P, Yoder A, Milleman J, Milleman K. Efficacy of Flossing and Mouthrinsing Regimens on Plaque and Gingivitis: A randomized clinical trial. J Dent Hyg. 2022 Jun;96(3):8-20. Erratum in: J Dent Hyg. 2022 Oct;96(5):5. PMID: 35654568.
Hung M, Patel H, Lee S, Nguyen J, Mohajeri A. The Influence of Vitamin D Levels on Dental Caries: A Retrospective Study of the United States Population. Nutrients. 2024 May 22;16(11):1572. doi: 10.3390/nu16111572. PMID: 38892506; PMCID: PMC11174693.
Disclaimer: This article does not represent medical advice, therefore please consult your doctor before using any products recommended here or following any suggestions in this article. This article is not sponsored by any company and contains affiliate links from which we may earn a small commission but at no cost to you, if you click on a product link.















What an exceptional piece of research. I’m going to watch the video go out and get some crust advanced and some Listerine and read this again on my big screen.
It’s amazing that this came to me right now because we have been challenged by teeth issues for a while and one of my daughters has dental anxiety.
Thank you so much.